
The Truth About Snoring and Sleep Disruption
Snoring is something most of us have encountered — either in ourselves or a partner — and it’s often brushed off as a harmless habit. In reality, snoring can sometimes be an early warning sign that your body is struggling to breathe properly during sleep.
While occasional snoring may simply result from a blocked nose, tiredness, or sleeping on your back, persistent or loud snoring shouldn’t be ignored. In some people, it signals an underlying condition known as sleep apnea, where breathing repeatedly stops and starts throughout the night.
These pauses can last for several seconds at a time, disrupting oxygen flow and preventing the deep, restorative rest the body needs. Over time, this can affect not only your energy levels but also your heart, blood pressure, and overall wellbeing.
What Happens When We Snore
Snoring occurs when the flow of air through the mouth and nose becomes partially blocked during sleep. As you drift into deeper rest, the muscles in your throat, tongue, and soft palate naturally relax. When these tissues loosen too much, they can narrow the airway and vibrate as air passes through — creating the familiar snoring sound.
The narrower the airway, the louder the vibrations tend to be. For some people, this happens occasionally, while for others it becomes a nightly occurrence. The sound itself is harmless, but it can indicate how freely air is moving in and out of the lungs.
Common triggers for snoring include nasal congestion, sleeping on your back, drinking alcohol before bed, exhaustion, and being overweight. These causes usually lead to temporary snoring — but when it becomes frequent or disruptive, it may point to something more serious affecting your breathing during sleep.
When Snoring Signals a Problem
Sometimes snoring isn’t just noise — it’s a sign that your airway is closing off during sleep. In people with a condition called sleep apnea, breathing repeatedly stops for several seconds at a time before the body jolts awake to reopen the airway. These interruptions can occur dozens, or even hundreds, of times in one night, often without the person realising it.
Each pause briefly cuts off oxygen to the body, forcing it out of deep sleep into lighter stages of sleep. As a result, even after a full night in bed, the person may wake up feeling unrefreshed and tired. This constant stop–start breathing places stress on the heart and prevents truly restorative rest.
The two main types of sleep apnea are:
- Obstructive Sleep Apnea (OSA): The most common type, caused by soft tissue in the throat collapsing and blocking airflow.
- Central Sleep Apnea (CSA): Less common, occurring when the brain temporarily fails to signal breathing muscles.
Though they arise for different reasons, both cause low oxygen levels, broken sleep, and strain on the body. Recognising these patterns early is key to preventing more serious health problems over time.
Signs You Shouldn’t Ignore

Not all snoring is cause for concern, but certain warning signs should prompt a closer look. If snoring is loud, persistent, and often commented on by a partner, it may be more than a minor irritation. Episodes of choking, snorting, or gasping for air during sleep are particularly significant, as they suggest the airway is repeatedly closing off.
Many people with sleep apnea also wake with a dry mouth, sore throat, or dull morning headaches. These occur when breathing through the mouth replaces normal nasal breathing, or when oxygen levels dip through the night. Even though the person may not recall waking, their body has been working hard to keep breathing.
Interrupted sleep takes its toll during the day. Persistent tiredness, poor concentration, or forgetfulness often follow, even after what seems like a long night’s rest. Some people notice increased irritability or mood swings, which can strain work or relationships. If several of these signs sound familiar, it’s worth speaking to a doctor or ENT specialist. Identifying and treating the cause early can restore quality sleep and prevent longer-term health complications.
Why It Matters
When sleep apnea is left untreated, the effects can reach far beyond disturbed rest. Each pause in breathing reduces oxygen levels and forces the body into a brief state of alarm, raising blood pressure and straining the heart. Over time, this repeated stress increases the risk of high blood pressure, irregular heart rhythms, and stroke. Research shows that people with untreated sleep apnea have a significantly higher risk of heart disease compared to those without it.
The condition also disrupts how the body regulates energy and metabolism. Poor sleep can interfere with blood sugar control and appetite hormones, making weight management more difficult and increasing the risk of developing insulin resistance or Type 2 diabetes.
Constant fatigue from broken sleep affects focus, memory, and alertness. Many people report nodding off during meetings or while driving, which can lead to avoidable accidents. These effects don’t appear overnight, but they build slowly, often unnoticed until health problems arise. Recognising and treating sleep apnea early can protect both your long-term well-being and your day-to-day quality of life.
Getting a Diagnosis
If you or your partner notice symptoms such as loud snoring, choking sounds, or excessive tiredness, an ENT or sleep specialist will begin by taking a detailed medical history. They may ask about your sleep habits, daytime fatigue, and whether anyone has observed pauses in your breathing. A physical examination of your nose, throat, and airway is also carried out to identify possible blockages or structural concerns.
To confirm a diagnosis, the specialist will often recommend a sleep study, known medically as polysomnography. This test records how your body functions during sleep, tracking breathing patterns, oxygen levels, heart rate, and brain activity. The information collected helps determine whether sleep apnea is present and how severe it is.
Results are usually expressed through an Apnea–Hypopnea Index, which measures how many times breathing stops or slows per hour: mild (5–14), moderate (15–29), and severe (30 or more). Understanding the severity is key to guiding the most suitable treatment, whether lifestyle changes, device therapy, or surgical options. With a proper diagnosis, effective management becomes possible — allowing sleep, energy, and overall health to recover.
Treatment and Management
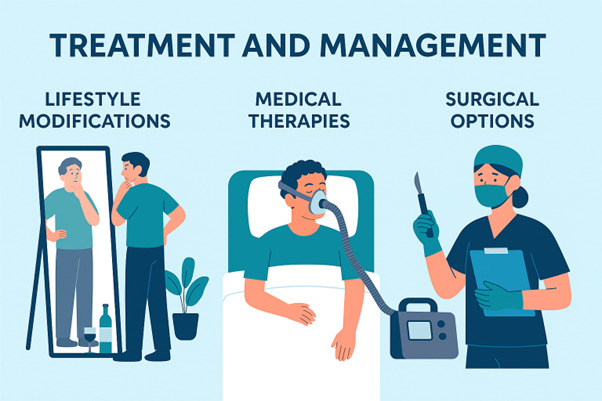
For many people, simple lifestyle adjustments can make a real difference. Losing excess weight helps to reduce pressure around the neck and airway, allowing for easier breathing during sleep. Avoiding alcohol or sedatives before bedtime prevents the throat muscles from relaxing too much, which can worsen snoring and apnea episodes. Sleeping on your side rather than your back also helps to keep the airway open naturally, particularly in mild cases.
If lifestyle changes aren’t enough, your specialist may suggest using a CPAP (Continuous Positive Airway Pressure) machine, which gently keeps airways open through a mask worn overnight. Custom-fitted oral appliances can also reposition the jaw or tongue to prevent collapse. CPAP isn’t a cure, but when used consistently, it effectively controls symptoms and prevents complications.
For patients with structural problems, surgery may be considered, such as removing enlarged tonsils, correcting a deviated nasal passage, or reshaping the soft palate. Surgery can significantly improve breathing and reduce symptoms, though results depend on individual anatomy. Every treatment plan is personalised to ensure the best long-term outcome.
When to Seek Help
It’s easy to dismiss snoring as an inconvenience, but when it becomes frequent, loud, or disrupts your sleep and your partner’s, it’s worth seeking medical advice. If anyone has observed you choking, gasping, or pausing in your breathing during sleep, these are clear warning signs that shouldn’t be ignored.
Persistent tiredness, morning headaches, or trouble concentrating can also indicate that your body isn’t getting the oxygen or rest it needs.
An ENT specialist is best placed to assess what’s causing your symptoms and determine whether it’s simple snoring or sleep apnea. They can examine your airway, arrange a sleep study if needed, and discuss treatment options suited to your situation.
Self-diagnosing or delaying a consultation can allow the problem to worsen over time. Untreated sleep apnea can contribute to serious health conditions such as high blood pressure, heart disease, and diabetes. Seeking help early not only protects your long-term health but also restores quality sleep — leaving you feeling more energised, alert, and focused throughout the day.
Closing Thoughts
Snoring might seem like a harmless part of sleep, but for many, it can be the body’s way of signalling that something isn’t quite right. When snoring becomes loud, persistent, or paired with breathing pauses and tiredness, it may be a sign of sleep apnea — a condition that deserves attention rather than avoidance. Recognising this early can make a lasting difference to your overall health and wellbeing.
Sleep apnea doesn’t just interrupt rest; it affects the heart, blood pressure, metabolism, and concentration. The good news is that with proper diagnosis and treatment, it’s a highly manageable condition. From lifestyle adjustments and sleep therapy to medical or surgical interventions, there are effective options available for every level of severity.
If you’ve noticed ongoing snoring or related symptoms, don’t ignore them or rely on guesswork. An ENT specialist can help identify the cause and create a treatment plan tailored to you. Taking that step not only protects your health but also restores the simple joy of waking up refreshed and ready to take on the day. Restful sleep isn’t a luxury — it’s an essential part of living well.
Frequently Asked Questions (FAQs)
1. Does severe snoring mean sleep apnea?
Not always. While loud or chronic snoring is a common symptom of sleep apnea, not everyone who snores has it. However, if your snoring is accompanied by choking, gasping, or pauses in breathing, it’s worth seeing a specialist to rule out sleep apnea.
2. How do you know if sleep apnea is serious?
Sleep apnea is considered serious when it disrupts oxygen levels or causes extreme daytime sleepiness. Severe cases — where breathing stops more than 30 times per hour — can increase the risk of heart problems, high blood pressure, and other complications.
3. What is the last stage of sleep apnea?
The most advanced form is called severe sleep apnea. In this stage, breathing pauses occur frequently throughout the night, significantly reducing oxygen levels. It can have a major impact on cardiovascular health and overall well-being if left untreated.
4. What is the root cause of sleep apnea?
Obstructive sleep apnea often develops when the muscles at the back of the throat relax excessively during sleep, blocking airflow. Other contributing factors include being overweight, having a narrow airway, nasal obstruction, or certain lifestyle habits such as alcohol use.
5. Can sleep apnea be cured completely?
There’s no universal cure, but many treatments effectively manage and reduce symptoms. Weight loss, CPAP therapy, oral appliances, and surgery can all help. With the right management plan, most people can lead healthy, well-rested lives.
